Summertime is busy for Rachel Reynolds, interim chief of dermatology at Beth Israel Deaconess Medical Center, on the clock and off.
Kris Snibbe/Harvard Staff Photographer
The social life of a dermatologist
It might be jarring when a complete stranger pulls up his shirt while you’re trying to eat dinner. It’s also an opportunity.
“Can I show you something?” comes the overture. Then the friend of a friend, second cousin, or complete stranger pulls up a hem, pulls down a collar, or just starts removing their clothes.
Such is the summer of the skin cancer expert. The season of beaches, barbecues, and picnics is also a period of awkward exposure, when the person whose name you don’t know really needs your opinion on this weird spot, never mind the appointment.
“With the skin, people can see the problem,” said Shadi Kourosh, director of the Dermatology Community Health Program at Massachusetts General Hospital and an assistant professor of dermatology at Harvard Medical School. “My colleagues can talk to their patients about heart disease and diabetes until they’re blue in the face, but that can fall on deaf ears because the person can’t see their heart disease and diabetes. But if they’ve got a spot and find out you’re a dermatologist, it doesn’t matter if you’re at a party or in an airline terminal.”


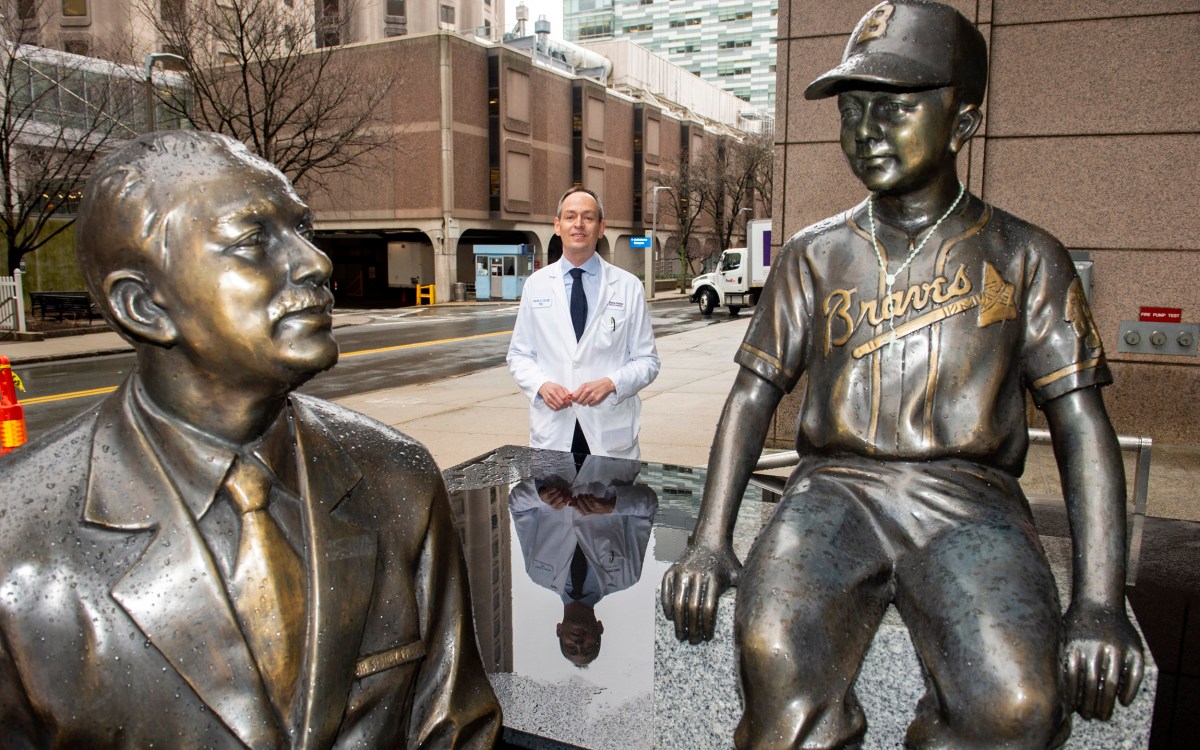
Elizabeth Buchbinder, a medical oncologist at the Dana-Farber Cancer Institute, and Shadi Kourosh, director of the Dermatology Community Health Program at Massachusetts General Hospital.
Photos by Kris Snibbe/Harvard Staff Photographer and courtesy of Shadi Kourosh
Among Kourosh’s most indelible encounters: the stranger at the airport who overheard her specialty and then yanked up his shirt to show her a blemish. Her Medical School colleague, Rachel Reynolds, also has stories to tell. The relatives who pull her into the bathroom for a quick scan. The houseguest who whipped off his shoes and socks to show her a wart on the bottom of his foot after walking Boston’s 2.5-mile Freedom Trail on a hot July day. But if the memories stick, she takes the questions in stride.
“That’s my job,” said Reynolds, interim chief of dermatology at Beth Israel Deaconess Medical Center. “We do get more requests for people to have things checked out in summertime. Families are out together and someone’s in a bathing suit and someone is seeing their back or some area that’s not obvious to the individual.”
“If they’ve got a spot and find out you’re a dermatologist, it doesn’t matter if you’re at a party or in an airline terminal.”
Skin cancer is the most common of all cancers. There are three main types: basal cell, squamous cell, and melanoma. Both basal and squamous cell carcinomas should be taken seriously, experts say, as either can metastasize. But mortality rates are relatively low — 2,000 deaths out of 3.3 million Americans diagnosed annually, according to the American Cancer Society.
Melanoma, which can spread rapidly throughout the body, is another story entirely. Though just under 98,000 diagnoses are expected this year, about 8,000 deaths are projected. Still, even as melanoma cases have risen in recent decades, advances in treatment have started to drive down death rates, giving experts like Elizabeth Buchbinder reason for hope.
“When I started in melanoma, a lot of doctors were like, ‘Why do you want to do melanoma? It’s the cancer that gives cancer a bad name,’” said Buchbinder, a medical oncologist at the Dana-Farber Cancer Institute and an assistant professor at the Medical School. “Everybody was dying with it. Now, over half our patients are still alive, six, seven years later, even with disease in their lungs, liver, brain.”
That transformation is what drew her to the field. Buchbinder did her oncology fellowship at Beth Israel when melanoma immunotherapy was just starting to produce dramatic turnarounds for extremely ill patients.
“It’s amazing science, it’s really interesting medicine, and it was an area where there was just so much we didn’t know and so much we had to learn that I got very excited and got involved in it,” she said. “I have just loved it because we have all of these new treatments and every day we’re learning more.”
While rapid treatment is crucial, prevention remains the most powerful anti-cancer weapon.
Mortality risk from a melanoma that is caught early can be as low as 5 percent, Buchbinder notes, but by the time the cancer has spread to the lymph nodes, the mortality rate goes up to 50 percent. Even with those odds, the prognosis has improved dramatically in recent years. In the past, patients would typically suffer a recurrence, often fatal. Today, immunotherapies can help doctors control advanced disease.
Another problem with melanoma is that tumors can increase in size in just the weeks it takes to schedule an appointment. That’s why Dana-Farber’s clinic has a 24-hour policy, where a patient is seen in a day’s time, and surgery is scheduled within a couple of weeks. It’s also one of the reasons experts don’t mind the occasional interruption at a birthday party or cookout.
“This is the job we’re supposed to do,” Kourosh said. “They have a spot on their skin and they’re losing sleep at night. It could be fine or it could be cancer, but they’re worried about it.”
While rapid treatment is crucial, prevention remains the most powerful anti-cancer weapon, experts agree. This means a sunscreen that protects against ultraviolet radiation, reapplied every two to four hours. It can also mean clothing — hats, shirts, and other items designed to deflect dangerous rays.
“The best medicine is the one the patient will use,” Kourosh said. “You have to sit down and get to know that person and figure out what is actually going to work for them and what’s realistic for them to adopt.”
Skin cancer typically stems from damage suffered early in life, but a middle-aged or older person retains power over their risk, she added.
“The exposure that a person got when they’re young can catch up with them, but that doesn’t mean that the story is over. When somebody comes to see me and they have that built up damage over a lifetime, oftentimes, as we treat them for precancers and skin cancers, and they adopt good, protective behaviors, I see over a period of years that their burden of skin cancer disease on their skin goes down.”