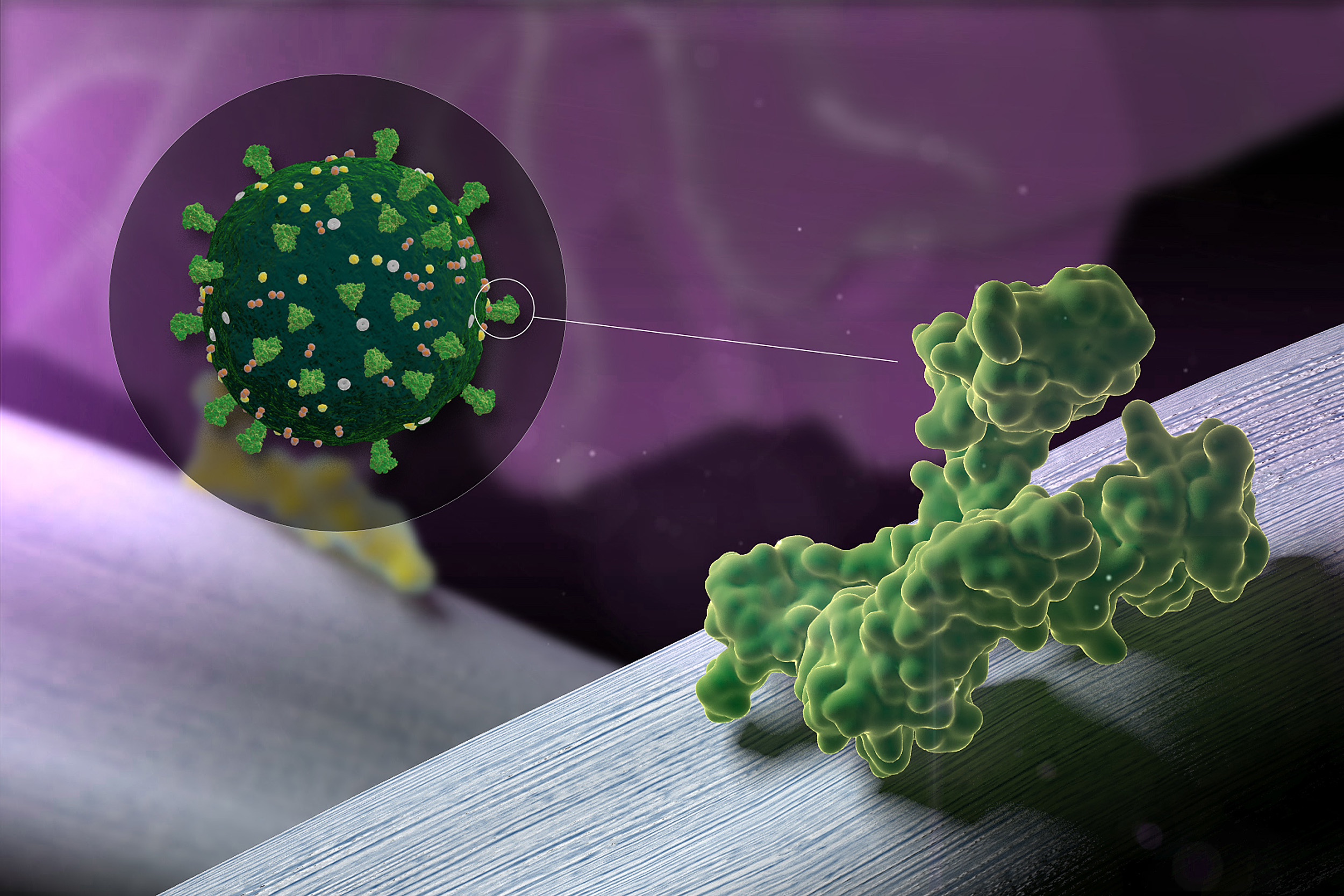
To create vaccine formulations against the SARS-CoV-2 virus, the team included combinations of different antigens derived from the virus’ Spike protein complex in the modular vaccine.
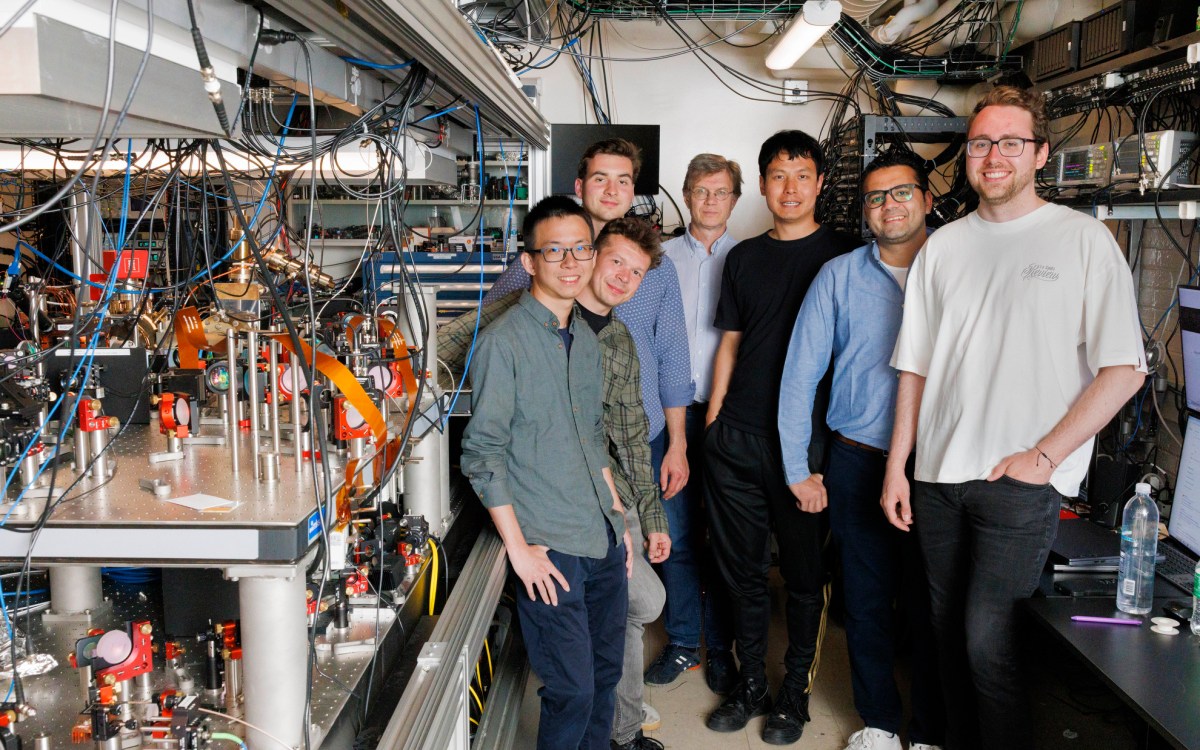
Credit: Wyss Institute at Harvard University
Putting a crown on OMNIVAX
The vaccine technology could be used in vaccines against SARS-CoV-2 and beyond
To confront the many challenges that infectious diseases pose to mankind head-on, a multi-disciplinary team of bioengineers, materials-scientists and immunologists at Harvard’s Wyss Institute has developed a broadly deployable biomaterials-based infection vaccine technology called “OMNIVAX.”
OMNIVAX was inspired by a fundamentally new cancer vaccine approach created by David Mooney’s group in the immuno-materials platform that he leads at Harvard’s Wyss Institute for Biologically Inspired Engineering. Mooney is a Wyss core faculty member and the Robert P. Pinkas Family Professor of Bioengineering at the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS).
The vaccine platform approach is rooted in the idea that antigens, when they are incorporated together with immune-activating adjuvants in a longer-lived biomaterial scaffold that concentrates immune cells at the site of vaccination, can be presented to the immune system in a more controlled and sustained way than when merely provided transiently in soluble form. As a result of this, the immune system’s protective responses can be more effective and prolonged.
Soon after COVID-19 started to spread across the globe, devastating a millions of lives and pushing the health systems and economies of many countries to their limits, Mooney’s team, which had previously focused on other infectious diseases, pivoted and used their OMNIVAX platform to generate vaccines against the SARS-CoV-2, the virus responsible for the pandemic.
It is widely accepted that a safe and effective vaccine that creates broad immunity against the coronavirus, and can be made quickly and distributed almost universally will be critical to address this pandemic. Experts estimate that it might take around 12 to 18 months to achieve this goal, which still would be record time for delivering a vaccine — and the race is on in many corners of the world.
The secrets of OMNIVAXination
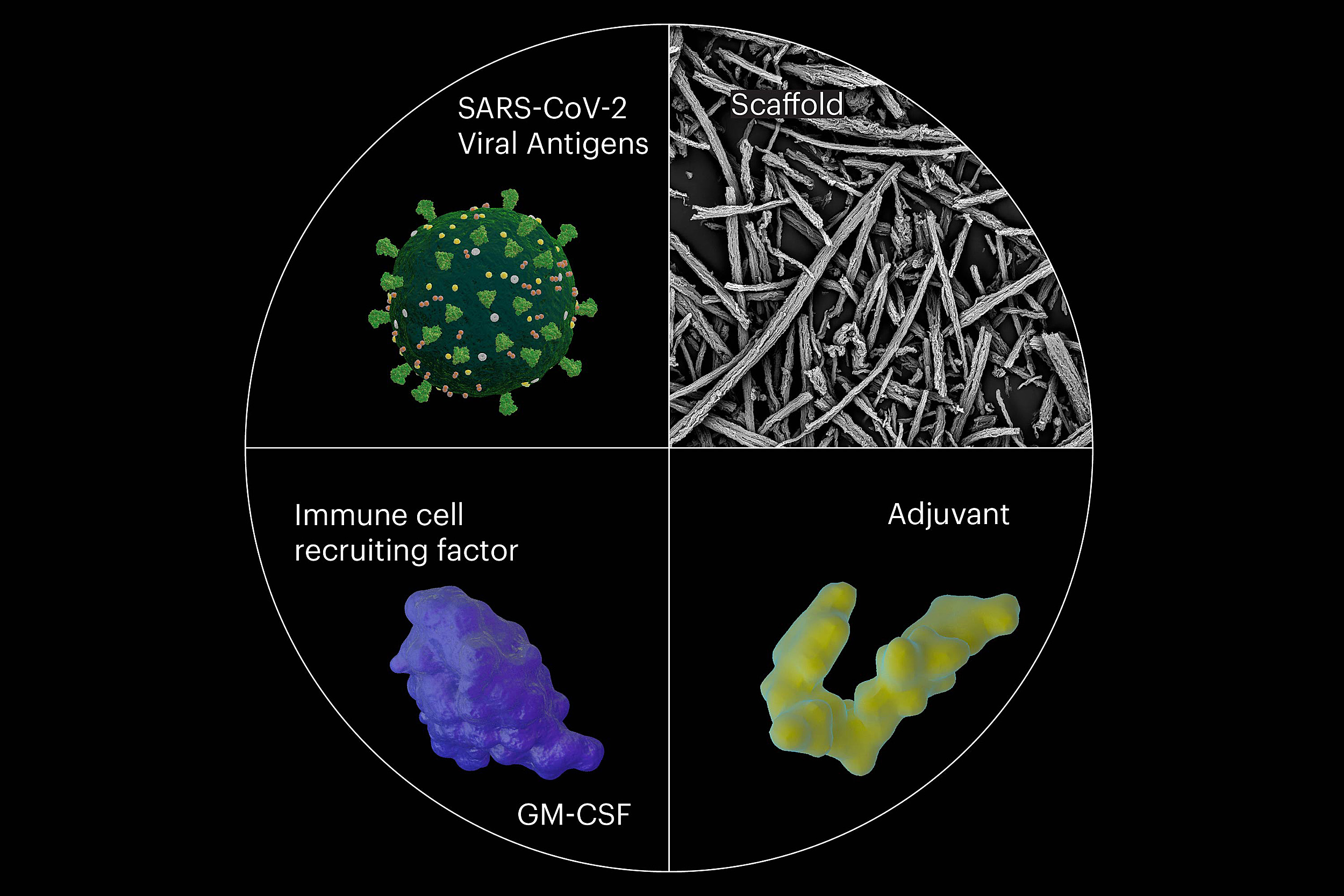
Using OMNIVAX’s fast and effective vaccine strategy, the team created a collection of vaccines against the COVID-19-causing SARS-CoV-2 virus. Their approach is highly modular, based on the simple and rapid combination of a mesoporous silica material, an adjuvant, the dendritic cell-recruiting factor GM-CSF, and one or more antigen(s). Many different antigens and adjuvants can be combined in a plug-and-play fashion.
The researchers believe that OMNIVAX vaccines with their unique structure and mechanism could provide protection against a number of infectious diseases caused by uncontrollable viral and bacterial pathogens, including those that will be responsible for forthcoming epidemics. Researchers believe it may have great potential to become a vaccine technology of the future.
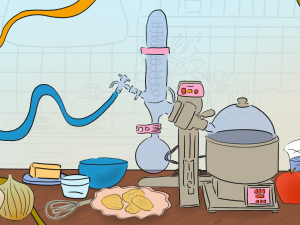
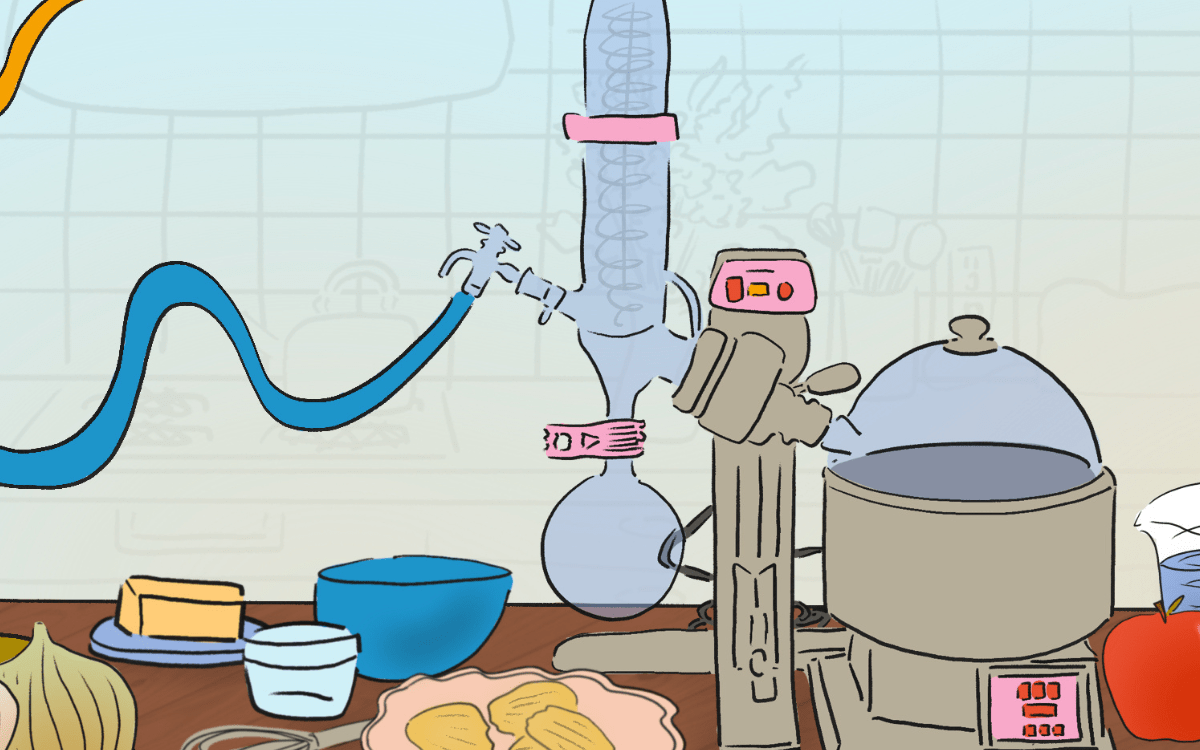
In the modular assembly of SARS-CoV-2-specific OMNIVAX vaccines, the team combined a scaffold-forming mesoporous silica biomaterial (top right), the dendritic cell-recruiting factor GM-CSF (bottom left), an immune-stimulating adjuvant (bottom right), and combinations of specific antigens derived from the host cell-binding spike structure on the surface of SARS-CoV-2 (top left).
Credit: Wyss Institute at Harvard University
The Wyss Institute recognized the potential of the technology early on, years before COVID-19 changed our world in a matter of a few months, and had designated the OMNIVAX platform technology “Institute Project” status. This prioritization is reserved for its most prestigious projects to accelerate their translational path to becoming the main assets of future startup companies with special business and technology development support.
The uniqueness of the OMNIVAX approach is based on its design that directs dendritic cells, the key orchestrators of pathogen-directed and other immune responses, to be actively recruited into the porous scaffold structure. Once in the structure, they are reprogrammed more effectively against a pathogen by specific antigen/adjuvant combinations. The trafficking of the dendritic cells can occur for the duration of the vaccine, allowing a significant multiplication of the resultant immune response.
Then, just like after their normal activation in the body, the reprogrammed dendritic cells migrate to nearby lymph nodes where they initiate a complex immune response involving both, fast-acting T cells and antibody-producing B cells that attack pathogens using different mechanisms. By allowing the activation of dendritic cells to be more prolonged, the OMNIVAX approach essentially adds a fourth dimension, namely time, to the three dimensions of the physical vaccine structure, which sets it apart from other vaccine approaches, and generates significantly more robust and durable responses than standard vaccines.
Vaccines against SARS-CoV-2 and beyond
Taking advantage of the modular nature of the OMNIVAX approach, the Wyss team generated their SARS-CoV-2 vaccines incorporating different combinations of viral antigens in combination with a general immune-activating adjuvant, and recently reported their preliminary findings in a bioRxiv paper. After receiving virus-specific antigens, it took the team merely three days to complete vaccines that were ready for injection.
A single injection of the vaccines into mice stimulated the rapid production of significant levels of antibodies that were specific to the viral antigens, and maintained for at least 96 days. In addition, the researchers analyzed blood sera from the vaccinated animals, the liquid component of blood which contains antibodies previously made by the immune system’s B cells like, in this case, SARS-CoV-2-directed antibodies.
More like this
In in vitro neutralization assays, the sera could prevent the infection of cultured cells by a SARS-CoV-2 pseudovirus, which is commonly used in coronavirus research as a key step to analyze the protective function of a vaccine. The team is currently pursuing studies in which they aim to protect animal models that are challenged with the actual coronavirus to confirm the efficacy of the vaccines.
Besides these first promising observations on the COVID-19 OMNIVAX vaccines, the team’s new approach could also provide protective solutions for many common unmet infectious diseases that have been threatening people in different environments.