
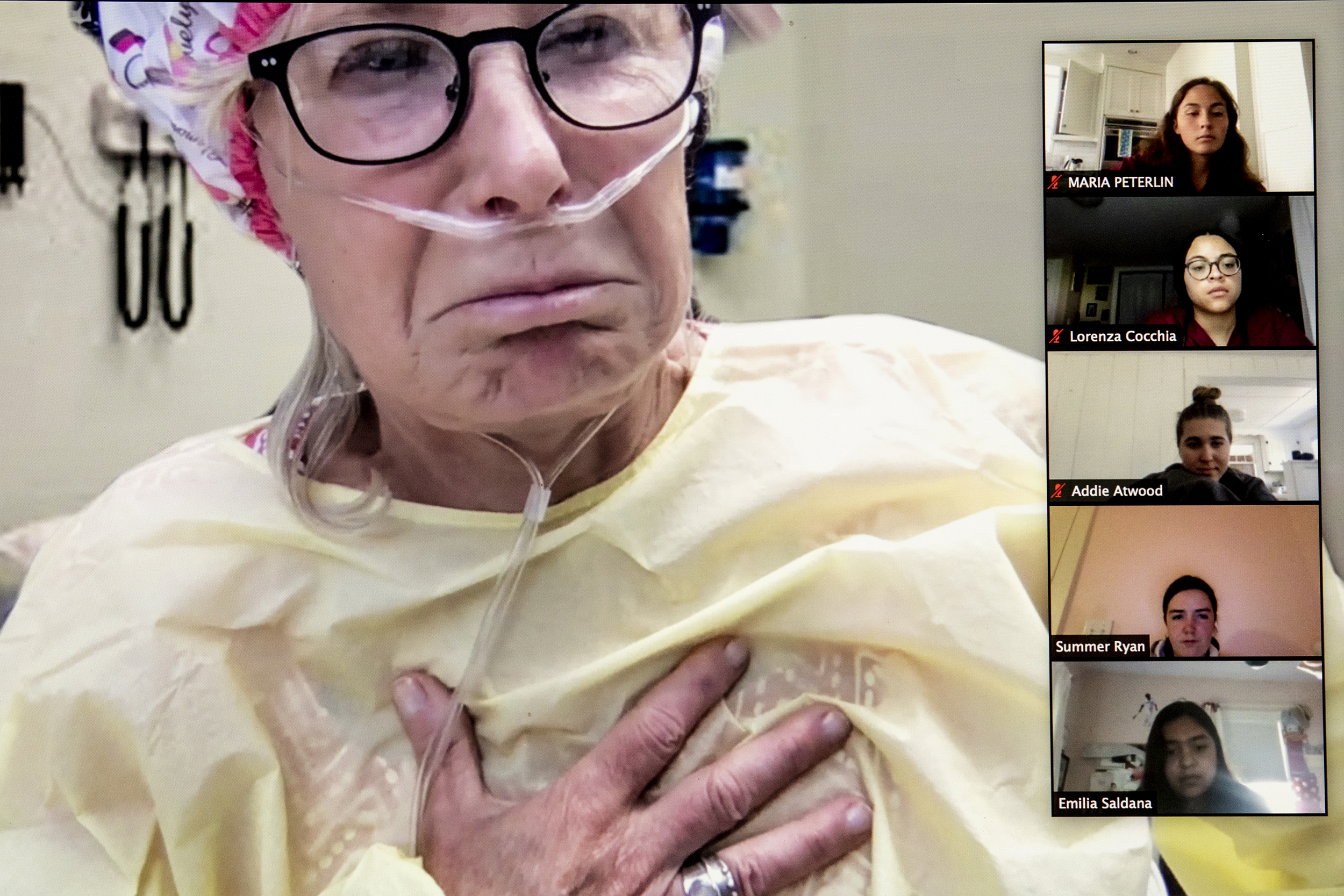
Harvard Medical School’s MEDscience Program Director Livia Rizzo talks with high school students following their diagnosis of a patient with fluid in her lungs.
Photos by Rose Lincoln/Harvard Staff Photographer
Medical immersion for students shifts online in pandemic
MEDscience program finds benefits to videoconferencing approach
When the patient went into cardiac arrest, more than a dozen high school students started CPR.
Urged on by a watching ER doc, the students didn’t let up until the patient, 78-year-old Bettie Smith, revived and sat up, to everyone’s relief. After all, it had been their recommendation she use an inhaler to ease the shortness of breath that had brought on the attack.
Together, the students, the ER doc (in reality an instructor for a 10-year-old medical education program called MEDscience), and Bettie (MEDscience’s executive director, Julie Joyal) encouraged and guided the students toward an appropriate diagnosis: heart attack due to a blocked coronary artery.
By the end of the hourlong simulation, Bettie was off to get a catherization that would ease the blockage that was robbing her heart muscle of blood and oxygen, and the students had a much better idea of a heart attack’s lesser-known symptoms and how a heart catheterization works.
“I really didn’t know what to expect … but it feels like real life,” said Maria Peterlin, a student at Boston Latin Academy with an interest in psychiatry. “It has definitely opened my eyes.”
For the last decade, Harvard Medical School’s MEDscience program has offered high school students a hands-on, case-based curriculum that covers the basic biology and clinical science needed to diagnose and treat a series of ailments. Along the way, it provides students with something of a tour of what can go wrong in the human body — heart attack, diabetes, addiction — as well as a glimpse of the power of modern medicine and the process through which it is wielded.
During the school year, HMS staff work with 40 high schools that have incorporated a MEDscience-designed program into their biology classes. The regular classroom instructors provide some 2,000 students with the basic scientific background every week before Joyal and Fiona Kennedy and Livia Rizzo present the hands-on cases, welcoming them to a mock examining room at HMS and introducing them to the stand-in posing as the patient.
Julie Joyal, executive director of the program, plays patient Bettie Smith in the ER with a medical condition that high school students resolve with help from an “ER doctor.”
The patient provides the symptoms, but it is the students who have to figure out the diagnosis. They are helped along by test results provided by the instructors, by their background scientific knowledge, and by their ability to consult and brainstorm with each other. The concept, according to Nancy Oriol, HMS’ associate dean for community engagement in medical education, is borrowed from the case-based instruction the School employs for medical students. A core feature is that participants are out of their depth, so there are no easy answers. That forces them to think critically, rely on each other, and act as a team.
“It’s not just ‘What’s wrong with the patient?’ it’s ‘How do you think your way through, how do you prove that’s it?’” Oriol said.
MEDscience closed in March, as did many other activities affected by COVID-19’s spread. As the weeks passed and it became apparent that that the pandemic would not allow the program to reopen for its weeklong, intensive summer version, Joyal and Oriol — whose brainchild the program was — began to think about other ways to offer an experience that had always been in person.
“It is really high-touch and hands-on,” Joyal said. “I didn’t think we’d be able to pivot.”
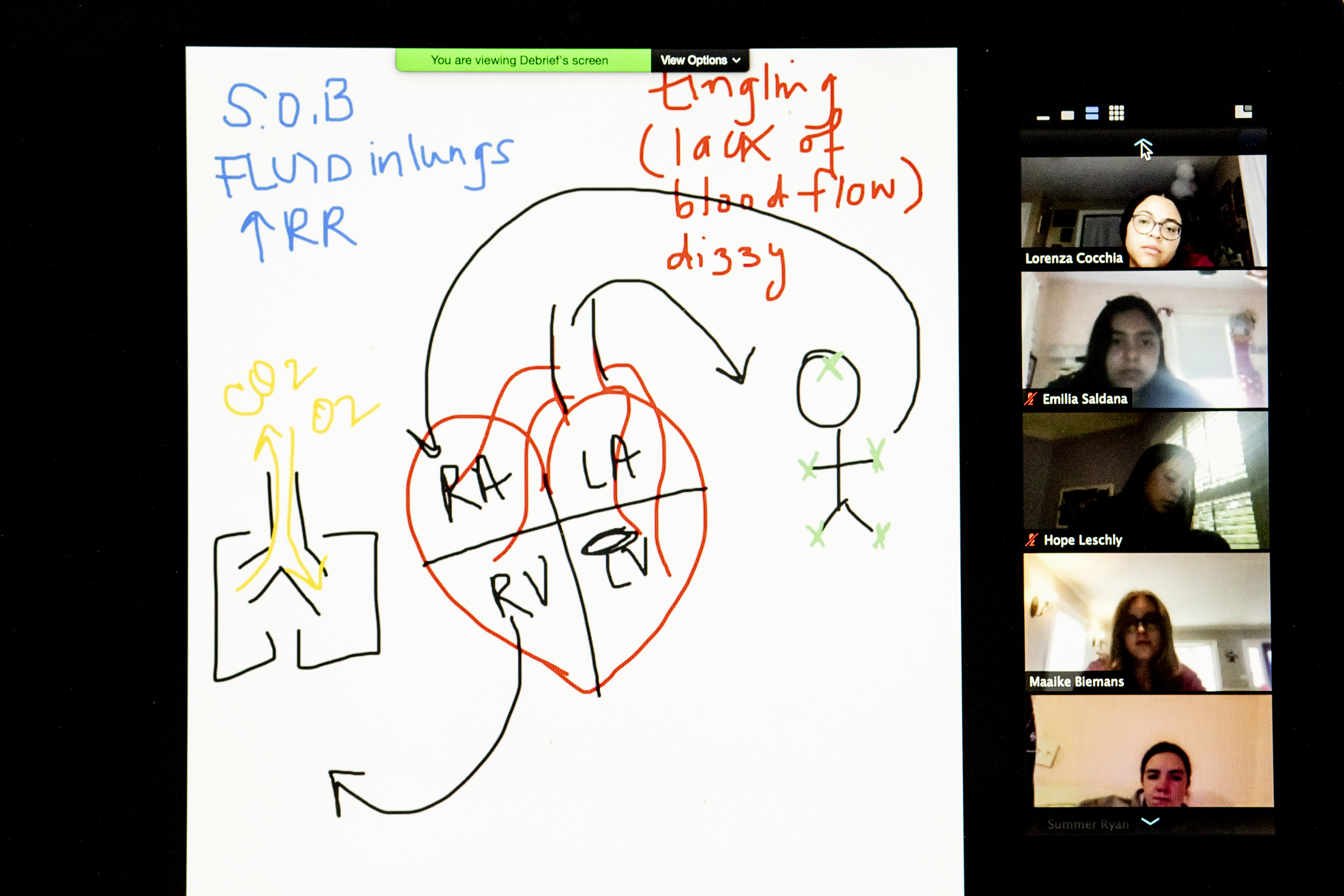

Patient information shared with the students.
But Joyal and Oriol realized that much would translate to a remote experience. The videoconferencing platform allows students to collaborate and brainstorm ideas, as they would in person. The scrubs and stethoscopes the program would normally hand out are easily mailed. And the experienced, energetic instructors would still ensure that students’ attention wouldn’t flag, as they pepper them with questions and draw in even the class’ quieter students.
“There is a mystery to solve with each patient and we want them to solve the mystery,” Kennedy said.
Oriol and Joyal also found the online format had unanticipated benefits. It forced them to exchange the medical training dummy they had been using for a human actor — Joyal — which gave students the ability to interview the patient directly and for Joyal to offer as much or as little information as needed. She can guide the students forward or stump them, forcing them to put their heads together and figure out another likely path. She can also give the students a jolt by flopping over mid-sentence, as she did in Bettie Smith’s mock heart attack.
A second benefit, Oriol said, is that the online format opens up the program to students far beyond Greater Boston.
“This is more than just making the best of a bad situation,” Oriol said. “This is a true silver lining.”
By mid-August, about 420 students had participated in MEDscience’s remote summer program, which for the first time includes students from around the world, including India, China, and Africa. In mid-August, Joyce Chisale, who will be entering Malawi College of Medicine in the fall, joined the class from her home in Malawi. Chisale said the course has provided her a first taste of what it might be like to be a doctor.
“When Bettie had a cardiac arrest I was totally shocked and the case felt realistic,” Chisale said. “It made me realize that when handling patients one can encounter unexpected cases which can be shocking, hence critical thinking will be needed.”
Oluwaseun Ogudimu, a high school student in Delaware, aspires to be a neurosurgeon and said the program has already given him a taste of what it’s like to make life-and-death decisions.
“We had to think quickly and respond quickly to save someone’s life,” Ogudimu said.
For some, like David Rodgers, a Georgetown University premed student serving as an intern this summer, the class’ effects are long-lasting. Rodgers said he was struck by the difference between the memorization-and-test learning strategy in traditional classes and the hands-on, problem-solving approach used by MEDscience.
“That’s what really kick-started my interest in the sciences,” Rodgers said. “What I had experienced was a lot of rinse-and-repeat in the classroom: Just learn material from a textbook. This program allowed me a different outlook, where you’re actually taking information … [and] using it in real life to solve a case.”
Oriol and Joyal said the online format offers MEDscience not just a way through the pandemic, but also an avenue for future growth. They had considered developing an online component before COVID, but it was a low priority. The pandemic forced them to rethink the program and adapt it into a format in which it has the potential for much broader reach.
“We’ve seen 420 kids this summer. I think it’s as effective as the hands-on program,” Joyal said.







