“I would like to see bisphosphonate tested prior to the arrival of a vaccine,” says immunologist Professor Uli von Andrian.
Image courtesy of Uli von Andrian
‘Faster protection with less material’
How a new vaccine adjuvant might eventually help to shorten the race to COVID-19 immunity
This is part of our Coronavirus Update series in which Harvard specialists in epidemiology, infectious disease, economics, politics, and other disciplines offer insights into what the latest developments in the COVID-19 outbreak may bring.
Uli von Andrian is the Mallinckrodt Professor of Immunopathology at Harvard Medical School and Program Leader of Basic Immunology at the Ragon Institute of MGH, MIT, and Harvard.
In an interview with the Harvard Office of Technology Development (OTD), von Andrian suggests that further research and development on a class of molecules called bisphosphonates might turbocharge a vaccine against SARS-CoV-2, the novel coronavirus, and help bring immunity to huge populations more quickly.
Q&A
Uli von Andrian
OTD: Hopefully, the first COVID-19 vaccines will be approved in the coming year or so, and the demand will be overwhelming. One of the challenges will be making enough doses to ensure herd immunity. How does your work address this challenge?
von Andrian: I remember when the swine flu hit the world. It turned out to be, fortunately, much less virulent than what we’re experiencing now. There was a vaccine developed relatively quickly. This was a flu virus, so there was a lot of technology already in place to make a vaccine for it. But I recall my kids and I trying to get this vaccine at the local high school. By the time we got there, there was already a line of people for a block and a half. And we actually never made it into the school, because they ran out of the vaccine way before it would have been our turn.
And I think the COVID-19 situation is at a completely different scale.
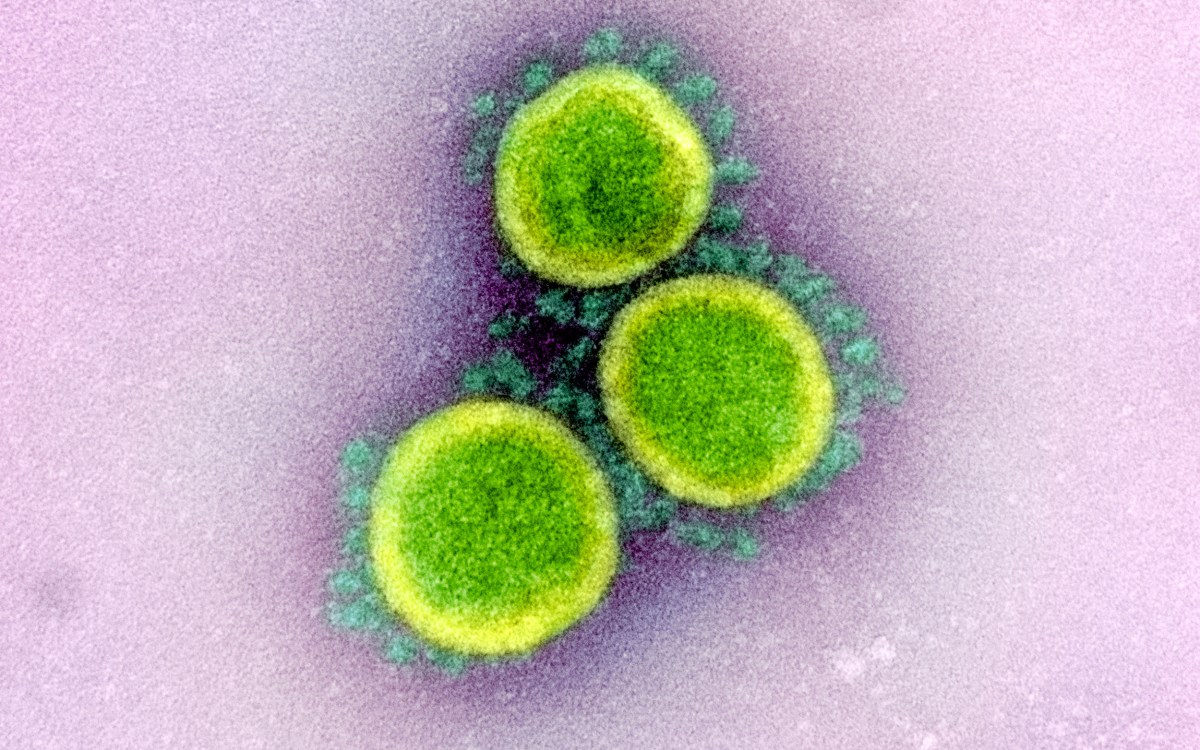
There are multiple vaccine candidates that all have one goal, I think, which is to enable patients to make neutralizing antibodies against a surface structure on the virus, the spike protein, which is composed of two subunits. The virus uses its spike to dock onto a target cell in a host and infect that cell. You can imagine, if you could gum this up with an antibody, this would prevent the virus from getting into the host cell. I think that idea is justified, because there are many other related coronavirus viruses where antibodies that target specific regions of the spike have been shown to be neutralizing.
OTD: So what’s the catch?
More like this
von Andrian: Well, there are multiple copies of this spike or protein on every single virus. So you need to make enough antibodies at sufficiently high affinity to detect and neutralize all of these spike proteins before the virus has a chance to get into a cell. The catch is that if you vaccinate someone and they start to make antibodies, it will take a while, often more than a month, to actually confer meaningful protection.
OTD: During an ongoing outbreak of disease, the need is more urgent. How can we speed it up?
von Andrian: We get help from adjuvants.
Imagine all the bacteria that live on our various surfaces that are completely innocuous. If we were to mount vigorous immune responses against every single one of those, our immune system would be completely overwhelmed. A lot of structures are molecularly boring to us and while they’re detected by the immune system, most of them are just ignored or tolerated, and for good reason.
If you have a misguided immune response against something that you should be tolerant to, you can get inflammatory diseases or allergies. So it’s important when you make a vaccine that the vaccine is provided in the proper context. It says, “Here’s a foreign structure, you actually need to pay attention to it, and this is the kind of immune response that you should raise against it.” This context is usually provided by what we call adjuvants, additives to the vaccine. Adjuvants can have very different chemical compositions, including lipids, proteins, nucleic acids, and even inorganic material, such as aluminum salt. They all have in common that they stimulate sensors in immune cells that are usually triggered by microbial infections or tissue damage.
So you can just say, “Watch out, it’s dangerous,” or you can yell at someone at the top of your lungs, “It’s dangerous!” And the response you will elicit will be different. The same can be said about the potency of adjuvants. The immune response you get will also differ, in terms of quantity and in terms of quality. Different adjuvants also trigger different sensing pathways in our immune system.
When you choose your vaccine antigens, you need to combine them with a sufficient danger signal.
OTD: So adjuvants are already used in vaccines. Does that not solve the problem for vaccines against the novel coronavirus?
von Andrian: There are a few promising vaccine candidates at the moment, including an mRNA vaccine and the work of Daniel Barouch at Beth Israel using adenoviral vectors, as well as others. But in most cases, you still have to wait weeks. The current trial for an mRNA vaccine, for instance, calls for a prime-boost protocol. That means you actually give the antigen, or the vaccine, twice, in a one-month interval.
The first time around, you alert the immune system. But in many cases, and that’s true for many other classic vaccines too, the response is not vigorous enough for long-lasting immunity to occur. You have to wait several weeks, and then this booster shot gives you the really vigorous antibody response that is much more longer lasting and of much greater quality. And then it’s typically yet another two weeks or so before you actually have protection.
So, whenever that vaccine is available, if you have to do to the prime-boost regimen before you get protection, you have to actually add another month and a half or so, on top of the date of the availability of the vaccine. So that’s what we can look forward to right now.
OTD: But you’ve made some important discoveries and innovations that could change the way vaccines are formulated.
von Andrian: Yes. We published it seven years ago, and we made the observation probably 10 years ago, that there’s a class of drugs called bisphosphonates that have some interesting adjuvant-like properties that were completely unexpected. This is what I think we should be looking into.
OTD: OK, walk us through it. What are these bisphosphonates, and how did you figure out they were useful here?
von Andrian: So these are small molecules, relatively simple drugs, actually, and widely used in the clinic. The first bisphosphonate was approved by the FDA in 1979 to prevent bone loss. There’s a whole family of small molecules that all have the classic core structure with two phosphorous groups. These are all very old drugs, so they’re generics, which means they are cheap and they’re widely available. One of the clinical uses is osteoporosis, because the osteoclasts that eat and destroy bone are selectively killed by this drug.
But bisphosphonates are also used experimentally in mouse immunology. You can package a bisphosphonate called Clodronate into a liposome — basically a tiny lipid bubble. To immune cells, to macrophages, they look just like a virus. But they kill off the macrophages, which lets you study the function of these cells in various disease models. It’s very useful.
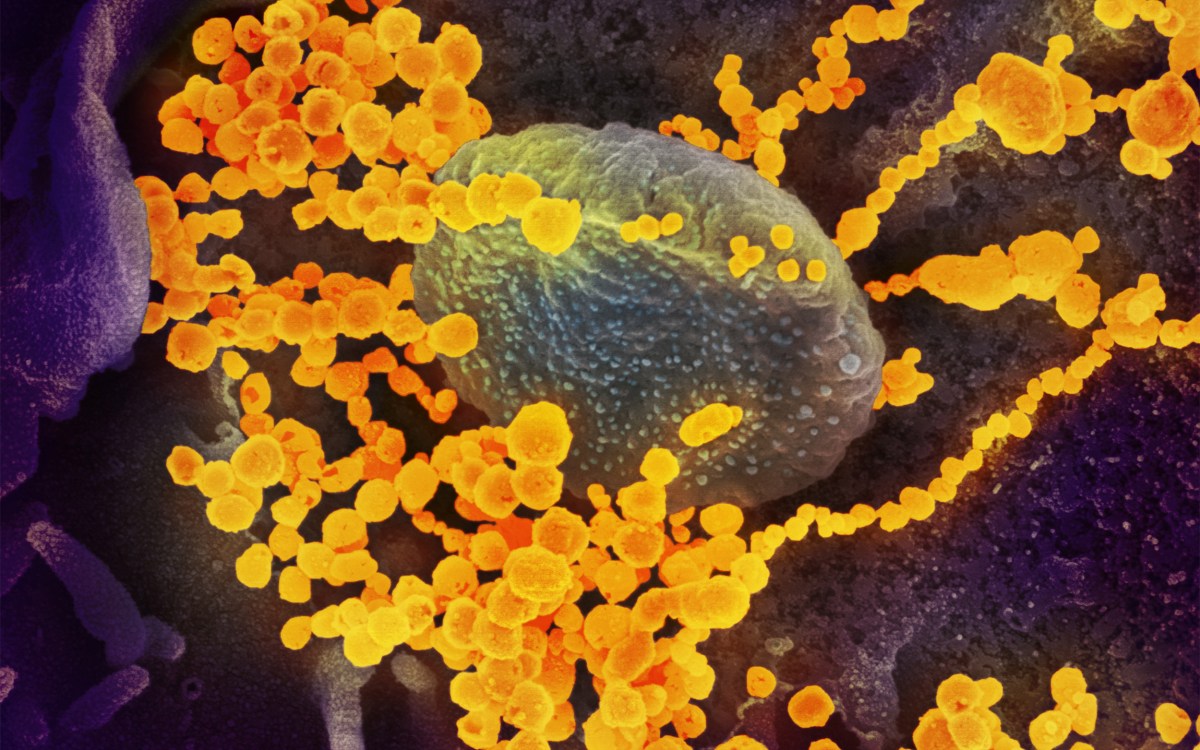
We were using these in my lab, and what we observed is that there’s a very specialized population of macrophages that live in the lymph nodes and initiate an immune response. These special macrophages capture viruses and present them to the B-cells so they can make antibodies. We published that in 2007. And we thought that if you deplete those macrophages with Clodronate liposomes, then it should have a negative effect on the mouse immune response.
But we were really surprised to see that the opposite happened. The immune response against the virus produced an antibody titer that was up to 100-fold greater compared to the control group. So that was weird. It suggested that maybe our findings were incorrect or our interpretation was not correct, and that actually these macrophages have the opposite function of what we had seen and what we had published. That troubled us a great deal.
It turned out that macrophages actually had nothing to do with it. When we gave Clodronate in free-form, which doesn’t deplete this group of macrophages, we actually saw the same dramatic effect on antibody responses.
Then, we said, aha, if this happens with Clodronate, perhaps it’s true for all the bisphosphonates. And so we tried several. And indeed, that’s what we saw. Each of the bisphosphonates we tested had this massive adjuvant-like effect, where the antibody response was much higher, but it was also much faster. We saw neutralizing antibody activity within just five days, at least for this Vesicular Stomatitis Virus that we were testing — very fast, after a single exposure.
So then we tried to figure out how this worked. We did a whole bunch of experiments that are described in this paper we published in 2013, which says that actually bisphosphonates have this additional and completely different mechanism of action.
OTD: In what way?
von Andrian: They do not work like any of the traditional adjuvants, but they seem to have a direct effect on B cells. For that reason, I think that they are really interesting. Because if you have an existing vaccine that already has an adjuvant that may be active, but perhaps weak, if you combine it with a bisphosphonate, you would expect to see synergistic activity. In fact, we tried bisphosphonate in combination with readily available vaccines, and we saw, indeed, that there was an amplification of the antibody immune response to those vaccines.
What we are now trying to explore in animal models is, could we basically use bisphosphonate to turbocharge whatever COVID-19 vaccines may come online, hopefully within a year or so.
OTD: In practical terms, how do you see it potentially improving the outcomes of vaccination?
von Andrian: The hope would be that by combining the vaccine with a bisphosphonate, you might need less vaccine per person. That means that if there’s a finite quantity that can be produced per unit time, you might be able to vaccinate more people. The second possibility is, by adding a bisphosphonate, perhaps a prime is enough and you don’t need a booster. So you could get much faster protection with less material.
OTD: That seems like it’s going to be so important if we want people to be able to return to normal life, or something like it.
von Andrian: Yes, absolutely, right. I’m hopeful. There’s quite a bit of information on bisphosphonate in humans. As far as I’m aware, I haven’t seen anything where people have looked specifically at immune responses, except actually in our own paper in 2013, but I think it’s really intriguing. And so personally, I would like to see bisphosphonate tested prior to the arrival of a vaccine.
OTD: What needs to happen next with this? Is the aim to move it into clinical trials? Who else needs to get involved in that effort?
von Andrian: I think to compel clinicians and regulatory agencies to agree to let us test this, I think we first need to do some more specific experiments with COVID-19 vaccines and with COVID-19 infection.
I have a subgroup of members of my lab who got special permission by the dean to actually go into the lab and do these experiments. Everyone else is supposed to stay at home. We have started to look at a few questions. The first one is to determine whether we can demonstrate in the lab that treatment for viral pneumonia with bisphosphonate is beneficial in mice. If so, what is the optimal dosing regimen? This is really important. Normally, bisphosphonates are used chronically over years. That’s not what we are talking about. We have to elucidate all these questions in animals first.
And then we’ve actually ordered several different bisphosphonates. They’re different in their chemistry and they’re different in how they’re administered. We’d like to compare them to see if one stands out as being particularly potent. That’s another important question.
Then separately and in parallel, we can address another question. If we immunize animal models at doses that are deliberately insufficient to elicit the maximum response, does the addition of the bisphosphonate give us an immune response that is equivalent to, or maybe better than the response to the vaccine alone at a higher dose?
And then what’s the quality and longevity of the immune response; what’s the onset of the immune response? In other words, can we replicate in primates what we’ve seen in mice? We will have to start in mice with the COVID-19 vaccine.
OTD: You mentioned that bisphosphonates have been around for a long time. Does that confer any advantage, given the urgency of these efforts?
von Andrian: That’s one of the beauties of this. They’re widely available and they’re generic, so they’re cheap. And they are already approved for clinical use. That’s actually very important, because there is no adjuvant that is approved anywhere as an adjuvant alone. There are only vaccines, where the vaccine is a combination of antigens plus an adjuvant. So that means if you have a candidate vaccine, it is what it is. You cannot just simply say, OK, as of today, I’m going to add a different adjuvant to it — unless there’s a drug that’s already approved for something else and, as the prescribing physician, you can use it off-label.
OTD: Are there certain collaborations that your lab group needs to build to make this happen?
von Andrian: Within my own group, I have very good people; they’re very experienced and eager to do this basic research. But as we move this along to other species, it will become extremely expensive. Then also, in particular, to take this from animals into the clinic will require expertise that others have much more than we do.
Being able to communicate and collaborate with all of the amazing members of our community is going to be absolutely critical to very rapidly move this out of the lab and into the clinic. That’s what we all hope for as scientists, right? In some way, you make a difference. And this would be, obviously, a wonderful way to contribute to this.
There’s so much at stake. And there are so many people that are going to suffer a great deal. I think as a member of humankind, you have an obligation to do what you can to deal with this in any way possible.