Unsplash
New blood test can detect wide range of cancers
Dana-Farber helps lead multi-center trial to provide testing results to patients for the first time
Editor’s Note: Enrollment in the PATHFINDER study is temporarily suspended due to the COVID-19 pandemic.
In a study involving thousands of participants, a new blood test detected more than 50 types of cancer as well as their location within the body with a high degree of accuracy, according to an international team of researchers led by Dana-Farber Cancer Institute, a Harvard affiliate, and the Mayo Clinic.
The results, published online today by the Annals of Oncology, indicate that the test — which identified some particularly dangerous cancers that lack standard approaches to screening — can play a key role in early detection of cancer. Early detection can often be critical to successful treatment.
Developed by Grail, Inc., of Menlo Park, Calif., the test uses next-generation sequencing to analyze the arrangement of chemical units called methyl groups on the DNA of cancer cells. Adhering to specific sections of DNA, methyl groups help control whether genes are active or inactive. In cancer cells, the placement of methyl groups, or methylation pattern, is often markedly different from that of normal cells — to the extent that abnormal methylation patterns are even more characteristic of cancer cells than genetic mutations are. When tumor cells die, their DNA, with methyl groups firmly attached, empties into the blood, where it can be analyzed by the new test.
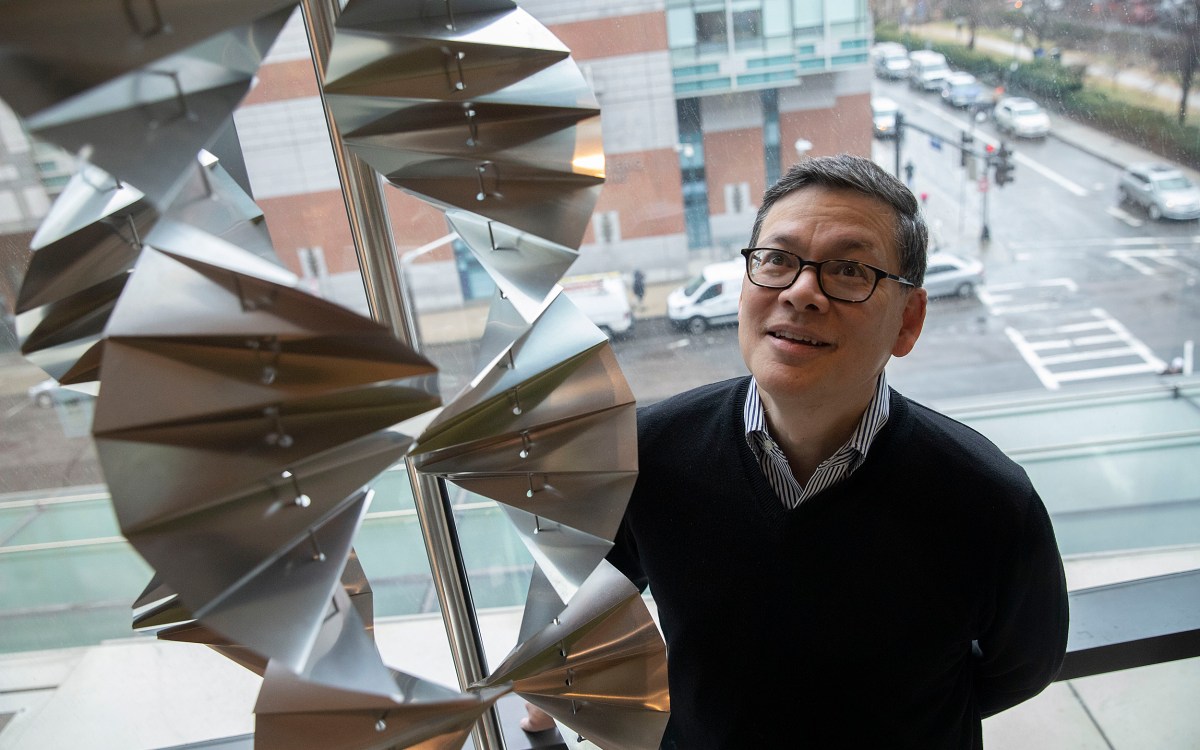
“Our previous work indicated that methylation-based tests outperform traditional DNA-sequencing approaches to detecting multiple forms of cancer in blood samples,” said Dana-Farber’s Geoffrey Oxnard, co-lead author of the study with Minetta Liu of the Mayo Clinic. “The results of this study suggest that such assays could be a feasible way of screening people for a wide variety of cancers.”
In the study, investigators used the test to analyze cell-free DNA (DNA from normal and cancerous cells that had entered the bloodstream upon the cells’ death) in 6,689 blood samples, including 2,482 from people diagnosed with cancer and 4,207 from people without cancer. The samples from patients with cancer represented more than 50 cancer types, including breast, colorectal, esophageal, gallbladder, bladder, gastric, ovarian, head and neck, lung, lymphoid leukemia, multiple myeloma, and pancreatic cancer.
The overall specificity of the test was 99.3 percent, meaning that only 0.7 percent of the results incorrectly indicated that cancer was present. The sensitivity of the assay for 12 cancers that account for nearly two-thirds of U.S. cancer deaths was 67.3 percent, meaning the test could find the cancer two-thirds of the time but a third of the time the test returned a negative result. Within this group, the sensitivity was 39 percent for patients with stage I cancer, 69 percent for those with stage II, 83 percent for those with stage III, and 92 percent for those with stage IV. The stage I-III sensitivity across all 50 cancer types was 43.9 percent. When cancer was detected, the test correctly identified the organ or tissue where the cancer originated in more than 90 percent of cases — critical information for determining how the disease is diagnosed and managed.
“Our results show that this approach to testing cell-free DNA in blood can detect a broad range of cancer types at virtually any stage of the disease, with specificity and sensitivity approaching the level needed for population-level screening. The test can be an important part of clinical trials for early cancer detection,” said Oxnard, an associate professor of medicine at Harvard Medical School.
The study was funded by Grail, Inc. As part of further validation research, Dana-Farber has joined a multi-center clinical trial of the test. The PATHFINDER study intends to enroll about 6,200 participants across the U.S. Participants in the study will have the results of the test communicated to them.